All new Macs come with the complete iWork suite for free. However, if you’re like me, and you have an aging (albeit fully functional, older Mac) then you need to pay full price ($20) for each of the the three iWork suites. However, thanks to our friends over at Redmond Pie, we now have a clever way of downloading the latest version of Numbers, Pages and Keynote for free–at least until Apple discovers and patches the exploit.
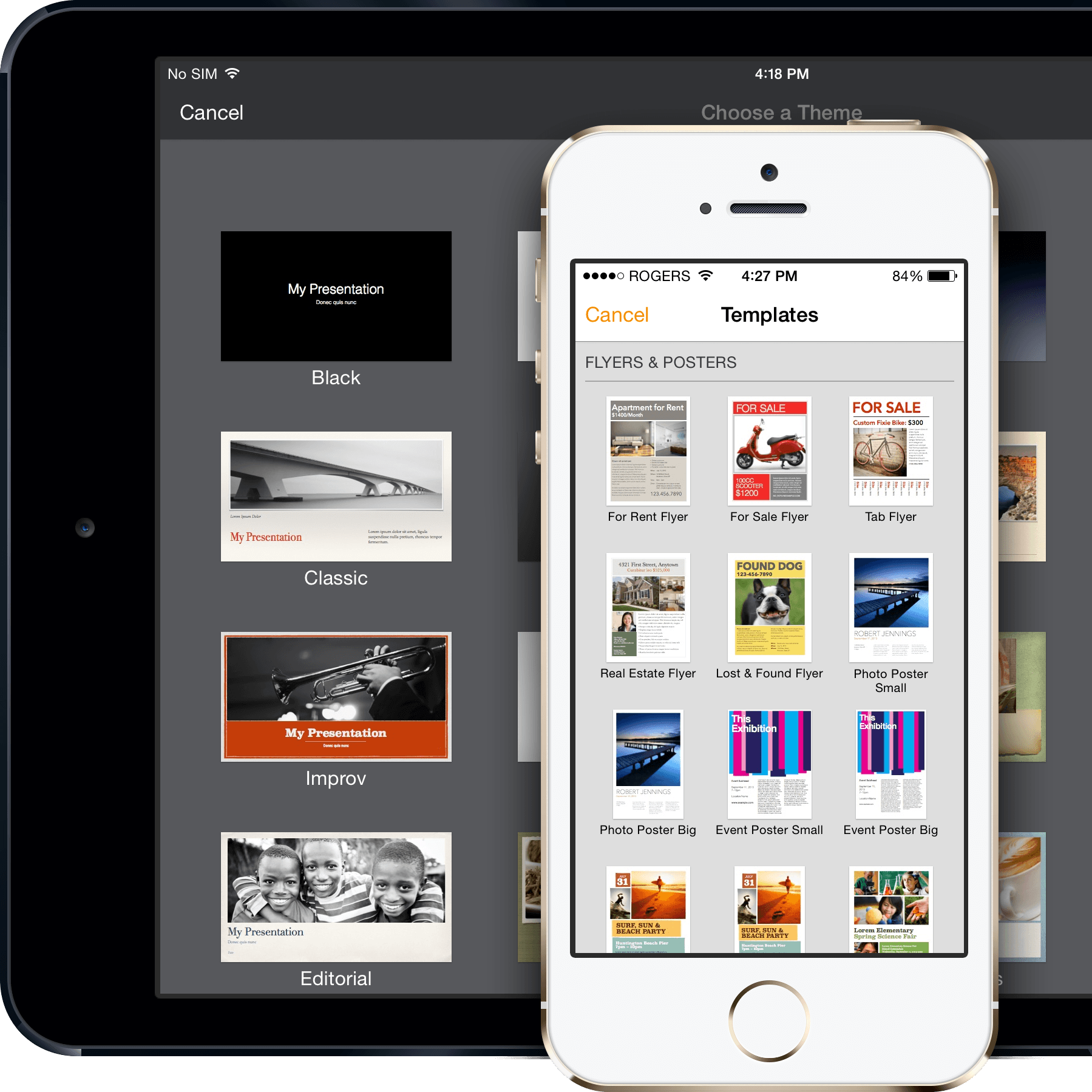
Numbers lets you build beautiful spreadsheets on a Mac, iPad, or iPhone — or on a PC using iWork for iCloud. And it’s compatible with Apple Pencil. Apple has released the latest versions of its iWork productivity suite today with 11.0 landing for the Pages, Numbers, and Keynote iOS and Mac apps. The new iOS builds feature support for precise. In 2014, after the release of the 2014 version of iWORK - The Missing Manual, I hoped that finally there would be in-depth information for word processing (not graphic design with text boxes) within the book. Keynote, at Tableau Conference 2014@theCUBE#Data14The data Wells Fargo collects, says Birtel, is mainly online click stream data on corporate banking custome. IWork is the easiest way to create stunning documents, spreadsheets and presentations. The release took place: August 22, 2014.
Until then, we’ve got you covered. I tried this last night, and it worked as advertised. I now have the most recent versions of the complete iWork suite and I can now download the update on any computer I have linked to the Mac App Store with my Apple ID.
Step 1-Download and install the iWork 09 trial.
Step 2-Launch Pages, Numbers and Keynote, and then quit each program.
Step 3-Open the Mac App Store and check the “Updates” tab for your updated version of each iWork app
Update each–relaunch, and you’re all set!
Let us know in the comments section below if it worked for you. Good luck!
Continue reading:

“Personalized Intraocular Pressure to Manage Glaucoma.”
Robert N. Weinreb, MD, Chairman and Distinguished Professor of Ophthalmology, and Director of the Shiley Eye Center at the University of California, San Diego, delivered the Glaucoma 360 - New Horizons Forum keynote lecture in San Francisco on February 7, 2014.
The Drs. Henry and Frederick Sutro Memorial Lecture, the keynote talk at New Horizons, features key opinion leaders and innovators in the field of glaucoma. 2014 was the first annual Sutro Lecture.
Lecture Transcript
Andrew Iwach, MD: Now it’s my honor to introduce something new to our meeting here today, the Henry and Frederick Sutro Memorial Lecture. This is possible as a result of a bequest of $3.2 million, which came to the Glaucoma Research Foundation over the past year. The bequest specifically asks that part of the funds be applied towards this meeting to support ophthalmic education, diagnostics and treatment.
Who was Henry Sutro? He was on the faculty at the University of Pacific. He was a very busy oral surgeon, loved photography, struggled with glaucoma and greatly appreciated the fact that to his last day, he could continue doing his photography, which was his passion.
His family is well known here in San Francisco. In fact, if you’ve heard of Sutro Tower, his great-grandfather was the former mayor. In fact, he owned a big chunk of the city back in the late 1800s. Our first annual Henry Sutro Frederick Sutro lecture is Dr. Robert Weinreb. We are so delighted. It’s so appropriate that he would be our first one.
A couple of words about Dr. Weinreb. He has an incredible background. He started in electrical engineering to MIT, Harvard for his medical degree, residency and fellowship here at UCSF. He's at the top at UCSD, really a world-renowned glaucoma specialist in charge of the Hamilton Glaucoma Center in San Diego.
He's led in many different areas. He's currently president of AGS Foundation as well as the Pan-American Glaucoma Society, but he's held top posts in all the major ophthalmic organizations in glaucoma, ARVO, AGS and the World Glaucoma Association.
His research is diverse and productive, a whole list of some of the different areas that he's been involved in, but I think what’s most important is his research has led to results, results that help patients but also provide us new tools so the rest of us can also take that step forward to help other patients.
Very involved in many areas, over 1,000 publications, 31 editorial boards, the list goes on. It was very hard for me in a few minutes to describe, to try to encapsulate the contributions that Dr. Weinreb has made. Bottom line, he’s a world-renowned clinician, surgeon, teacher and scientist. With that, I’d like to ask Dr. Weinreb up. As our first annual recipient, we have a plaque to commemorate his presentation here today.
Robert N. Weinreb, MD: Thanks Andy. Congratulations to Dr. Iwach, Dr. Graves, the Glaucoma Research Foundation and Tom Bruno for this extraordinary three days that they’ve put together with the wonderful event last night, the meeting this morning and the meeting tomorrow. It’s a great honor for me to deliver the inaugural Sutro Lecture.
Given that this is an innovation meeting, I will talk about something that I believe will be disruptive for glaucoma and transformative for our patients, namely personalizing intraocular pressure to manage glaucoma.
Disclosures: I consult and receive research support form a number of groups, including several who have activities relating to the space.
Today in clinical practice, most clinicians will see their glaucoma patients or glaucoma suspects perhaps once or twice a year. They obtain an intraocular pressure in their office, and based on that single reading, they might adjust treatment, or they might suggest the patient return in another year.
If they adjust treatment, they might see the patient again a couple of months later. Such glaucoma patients may be seen three or four times during the year with single measurements of intraocular pressure.
Is there a problem with that? One problem is that the single intraocular pressure assessment in the office might actually just capture the peak intraocular pressure. This would allow you to adjust your treatment based on peak intraocular pressure, something that very plausibly could be related to glaucoma damage.
However, the real IOP might be higher. In fact, during those snapshots of intraocular pressure that are obtained in the office, you might miss the higher intraocular pressure that occurs at other times during the day. The real high IOP in that case would be undetected, and the management decisions that you make or more likely wouldn’t make might not necessarily benefit the patient.
Intraocular pressure measurements are complicated by the fact that intraocular pressure can vary from moment to moment. It can vary over seconds. It can vary over minutes. It can vary over hours.
In fact, we don’t even know whether it is a single intraocular pressure reading such as the peak IOP, which is used by most clinicians for decision making, mean intraocular pressure, the parameter that has been most extensively characterized in a large number of clinical trials or the fluctuation of intraocular pressure that is most meaningful.
Fluctuation of intraocular pressure in particular is quite interesting because there are so many conflicting data with many types and multiple ways to analyze. There are short-term variations of intraocular pressure that can occur over days or weeks, and there’s long-term fluctuation of intraocular pressure that can occur over months, seasons or even years. What is a clinician to do to help our patients?
It is even more complicated by the fact that intraocular pressure is not conserved from day to day. Intraocular pressure at specific times on a given day does not provide meaningful information regarding intraocular pressure at same times on other days.
Here are two patients from a study by Tony Realini in which you can see in blue, intraocular pressure on one day, and in pink, intraocular pressure on another day. Depending on the day, the right eye might be higher on one day and lower on another day. It is not conserved from day to day.
You cannot assume the pressure at the same time on different days will be the same, something that is a basic assumption made for the one-eyed therapeutic trial. This is one reason why the one-eyed therapeutic trial simply does not work in clinical practice.

How can one understand better this conundrum of the changing intraocular pressure? Steady-state intraocular pressure depends on the rate of aqueous formation, the facility of outflow and episcleral venous pressure. This is the Goldman equation. It has a circadian rhythm, which means it changes throughout the day. As mentioned before, you it is not the same from day to day.
Almost 20 years ago, with John Liu at UCSD, we established a sleep laboratory to investigate habitual intraocular pressure. Habitual intraocular pressure is pressure in the positions of habit, which for most of us is sitting or standing during the day and supine during the evening.
One of the most striking findings that we found in our first patient and has been consistent throughout our studies, in about two thirds of our patients, is that intraocular pressure is not highest during the day, but highest at nighttime.
The nocturnal pressure is highest at night in healthy individuals. It's highest in glaucoma individuals. It’s not only higher because of the supine position at night. In fact, if you take intraocular pressure in patients who are supine over 24 hours, intraocular pressure in healthy individuals and individuals with glaucoma is still higher during the nighttime.
This was surprising because as I will show you shortly, aqueous flow is lowest at nighttime. We haven’t understood why intraocular pressure would be highest at night when aqueous flow is lowest.
These data introduced a controversial question. Can adjusting body position to lower pressure minimize glaucoma progression? If intraocular pressure is higher in a supine position than in a sitting position, would raising the head of the bed to make a difference in glaucoma progression? It is clear that the intraocular pressure would be lower, but is that sufficient to reduce progression?
Intraocular pressure also increases in flexion and extension. Are extra pillows detrimental? I also will show you some information that suggests we still don’t know what we can do with regards to this. Then intraocular pressure increases in the lateral decubitus position, which means when you lie on a side, the dependent eye, the eye on the bottom is higher. Could this contribute to glaucoma asymmetry?
Even though intraocular pressure is lower, when you go from a supine position to a head-up position, there are other physiologic parameters that change, including perfusion pressure, blood pressure and also intracranial pressure.
Perfusion pressure is the difference between blood pressure and intraocular pressure. In a number of large studies, perfusion pressure has been shown not only to be a risk factor for glaucoma and glaucoma progression, but low perfusion pressure is a more powerful risk factor for developing glaucoma and a more powerful risk factor for progressive glaucoma than intraocular pressure.
If you have low perfusion pressure, your risk for glaucoma and glaucoma progression is increased. When you take someone from a supine position and elevate the head of the bed or put an extra pillow, not only are you changing intraocular pressure, but you are changing perfusion pressure.
Let me give you an example, and this is from Arthur Sit, who conceptualized the intraocular pressure readings that we obtain in our patients. Typically, you’re seeing here intraocular pressure going down during the day. Then at nighttime, intraocular pressure increases. Then upon awakening it goes down again.
At the same time, if you look at blood pressure as we have in our sleep laboratory, , whether diastolic or whether systolic, it is lower at nighttime. Higher during the day, exactly opposite to what you is seen with intraocular pressure.
What does that mean for perfusion pressure? Perfusion pressure is lowest at nighttime. Is it possible that glaucoma progression is occurring at nighttime when perfusion pressure is lowest? In fact, you can calculate the perfusion pressure in different body positions using some measurements that have been provided by a number of investigators.
Perfusion pressure, not only blood pressure, is lowest in a supine position. Intracranial pressure also changes. There is exciting new work showing that glaucoma and glaucoma progression may depend not on intraocular pressure, not on perfusion pressure but on trans-laminar pressure, which is the difference between intraocular pressure and intracranial pressure.
Taking the fact that intraocular pressure is highest at nighttime and in a supine position and simply saying to a patient, “Elevate the head of your bed, sleep on an extra pillow,” might in fact be doing harm for a patient. Now, there are other things that one can do though to reduce intraocular pressure over 24 hours.
Let’s go back to, again, some basic physiology. This is brilliant work done by Brubaker 20 years ago. He looked at the 24-hour rhythm of aqueous humor formation and flow. In brief, what he found was that aqueous flow was highest in the morning between 6:00 a.m. and 12:00 noon. Over a six-hour period, which represents 25 percent of the day, there is about one third of our aqueous flow, a rate of about three microliters per minute.
At nighttime, the nocturnal period, an eight-hour period between 10:00 p.m. and 6:00 a.m., aqueous flow is lowest, 1.2 microliters per minute. Over this period that's one third of the day, there only is about one sixth of our flow. The dilemma has been if aqueous flow is so low at night, how could intraocular pressure be high at night?
One of the questions that I was asked over the last two decades when I talked about this topic is do I think it might be an artifact, the fact that intraocular pressure is highest at nighttime because we know that aqueous flow is lowest.
Now, this is true not only in healthy individuals, but it is also true in individuals who are ocular hypertensive. It's also true in individuals with glaucoma. The question about how could be flow be lowest and pressure highest was recently addressed in important work done by Arthur Sit at Mayo. Dr. Sit inherited the Brubaker laboratory, and he used a variety of techniques, including a fluorophotometry method developed by Brubaker and his own method to measure episcleral venous pressure.
If Dr. Sit confirmed that intraocular pressure is lower at nighttime. He measured intraocular pressure in a sitting position. If you look at facility, which largely is a measure of the trabecular meshwork, it is unchanged, but he observed that uveoscleral flow goes down at nighttime.
We see no change when you are solely in a sitting position in episcleral venous pressure from day to night. There is a small decrease in outflow facility. However, the change in uveoscleral flow largely accounts and compensates for the decrease in aqueous humor production rate to keep intraocular pressure from decreasing at night.
This brings up a whole new group of therapeutic possibilities and also helps us understand some of our current therapies for lowering intraocular pressure. When you examine the four major classes of drugs that we use, carbonic anhydrase inhibitors, alpha agonists, beta-adrenergic antagonists and prostaglandin analogs, we recognize that each one of them has a very characteristic mechanism of action.
The beta blockers and the carbonic anhydrase inhibitors both reduce aqueous humor formation. The alpha agonists are said to have a dual mechanism. Initially they reduce aqueous humor formation and then may have an effect on uveoscleral outflow. The prostaglandin analogs increase outflow, probably most through the uveoscleral outflow pathway.
Iwork
Now, given these very distinct mechanisms of action, it was reasonable to expect that they might have differential effects on 24-hour intraocular pressure. In retrospect, now that we know that the uveoscleral outflow is lower at nighttime, we can see that these drug classes should have distinct actions.
This is a series of studies conducted with John Liu in our sleep laboratory in which we looked at how do the classes of drugs affect the 24-hour intraocular pressure. We bring patients into the sleep laboratory and obtain a baseline. This is a typical pressure curve. This is a mean of many patients. Then we randomly assign them to drug A or drug B.
This particular study was is a randomized crossover design with a beta blocker and a prostaglandin analog. Each was used for a month. We bring them back into the sleep laboratory. We measure their intraocular pressure over 24 hours. They obtained drug A then drug B. If they obtained drug B first by random selection they then next received drug A.
We found that beta blockers are very effective drugs during the day but had no pressure lowering effect at nighttime. In fact, you can argue that not only is intraocular pressure not reduced at night, but blood pressure and perfusion pressure are reduced. Is Timolol a drug that you would want to treat yourself or a family member if it’s reducing your perfusion pressure at nighttime?
Prostaglandin analogs are very different as they are effective during the day, in fact a little more effective than the beta blockers, and also very effective at night. They do not have an effect on blood pressure or perfusion pressure. They are our first line of therapy.
The alpha-agonists, brimonidine, was effective during the day, and had no effect on intraocular pressure at night. Experimentally, it has neuroprotective effects. In one study, the LOGIT study, it may have been more effective than timolol in preserving visual field.
In another study, we investigated only patients who were on a topical prostaglandin analog, brought them into the sleep laboratory, and examined whether a carbonic anhydrase inhibitor or beta blocker was a more effective second line therapy.
We added a beta blocker or a carbonic anhydrase inhibitor, brinzolamide. When added to a prostaglandin, the beta blocker not surprisingly did not lower pressure at nighttime, whereas the carbonic anhydrase inhibitor was effective during the day and night, very much like a prostaglandin analog.
You have two classes of drugs, prostaglandin analogs and carbonic anhydrase inhibitors, that are effective during the day and during the night. Neither one of them affects perfusion pressure or blood pressure. Each of the classes of drugs that we currently use for treating glaucoma have a distinct mechanism of action, and each of the classes of drugs that are under investigation also have a distinct mechanism of action.
I would opine that we will learn that the drugs that lower intraocular pressure over 24 hours and do not lower perfusion pressure will be preferred. Unless, of course, a drug does not have an additional effect, maybe neuroprotection or maybe vasodilation to enhance blood flow to the optic nerve. Laser trabeculoplasty is also effective at lowering pressure during the nighttime. How can these results be applied in clinical practice?
The future is 24-hour monitoring of intraocular pressure. That’s the transformative event. That will be a huge disruptor in the glaucoma space.
There are two approaches, temporary and permanent continuous measurement.
The Sensimed Triggerfish, developed by Leonardi, is a temporary approach. With the first patient that we studied with this technology, intraocular pressure was highest at nighttime, confirming the 20 years of sleep laboratory work that we did. Pressure is highest at nighttime in two thirds of our patients. With trabeculectomy, intraocular pressure is lower during the day and during the night, just like a PGA and a CAI, topical CAI.
With another subject, pressure is lower at nighttime than during the day. Why is that? This is an airline pilot. His 24-hour cycles are off. This technology is approved in Europe and there are issues of cost reimbursement. Moreover, it does not measure intraocular pressure directly. It measures change in corneal curvature, and corneal biomechanics might have an effect.
Other technologies include the implantable intraocular pressure monitors. Implandata has developed an exciting technology that uses an application-specific integrated circuit with temperature sensors, and pressure sensors to measure intraocular pressure. It is being used in clinical trials now in K-Pro patients. It also is being studied in patients undergoing cataract surgery in Europe.
At this time there’s no continuous pressure model available for clinical use in the U.S. The temporary measurement with the contact lens is non-invasive. For the absolute intraocular pressure measurement, permanent monitoring with an implantable device is going to be a more effective solution than the temporary one with the contact lens.
Iwork 2014 Dmg
With large amounts of data on 24-hour pressure, new analytic methods will be needed for analysis, such as machine learning. One then should be able to refine and individualize target intraocular pressure. We should learn whether it is the peak intraocular pressure, the mean intraocular pressure, or the fluctuation that matters most. More importantly, drug delivery devices and surgical techniques will be integrated with IOP lowering, so we should be able measure intraocular pressure perhaps with the same device that we use to regulate it with drugs or surgical devices.
Iwork 2014 Full Mega
To summarize, a single measurement of intraocular pressure during usual office hours is insufficient. Intraocular pressure is usually highest at night. Clinicians can maximize the value of office intraocular pressure by obtaining measurements at different times of the day and obtaining as many intraocular pressure measurements as possible.
The selection of therapy can help lower 24-hour intraocular pressure and minimize variability. We need to consider nocturnal intraocular pressure elevations and positional dependence. However, how we do that is still unclear.
Iwork 2014 Download
24-hour intraocular pressure monitoring is needed to fully elucidate the importance of circadian intraocular pressure. Much of the information that I talked about today is presented in greater detail in the World Glaucoma Association Consensus on Intraocular pressure published by Kugler Publications.
In conclusion, 24-hour intraocular pressure monitoring offers potential for personalizing intraocular pressure for optimal glaucoma management. It will be transformative for patient care. There will be a plethora of data to provide a much deeper insight into patient management with glaucoma.
I want to acknowledge my collaborators who have worked with me on many of these topics. Thank you. It has been an honor to deliver the inaugural Sutro lecture.
End Transcript
